What Won’t Change? Part Three: Payer Experience
Insurance companies hold significant influence over cost and quality in the modern health care system. Here’s how payers will continue to shape health care in the United States.
This is the final installment of a three-part series called “What Won’t Change?” where we examine the mainstays in health care that are likely to stay the same over the next decade.
1. Spending will remain unsustainable
All of the ways we measure health care cost and spending in this country show an unrelenting upward trajectory, one that has persisted for decades. Reversing them would be like trying to reverse a train with an infinite fuel supply and bad brakes.
A 2020 Brookings Institution report shows that, as a share of gross domestic product, health care accounted for about 10% in 1987, including public and private insurance and out-of-pocket expenditures. In 2018, health care’s share of GDP nearly doubled to 18%.
At the individual level, spending per capita swelled from about $4,500 in 1987 to $11,000 in 2015, according to Brookings.
Combined, those metrics reveal the cost per person is growing rapidly while it gobbles up a greater share of total consumption and spending in the United States.
Underscoring the data, we know that the population is growing older and will continue to get sicker.
Calling something “unsustainable” assumes it will collapse eventually. Realistically, we will not see a complete disintegration. Instead, we will continue to find ways to glue it together. Taxes and premiums will rise. People will spend more of their earnings. Innovation will grow more costly. The quality of care will diminish.
On the margins, people who can’t afford care will take what they can get or, in some cases, simply go untreated. The latter only drive up costs more when they end up in the emergency room with untreated chronic conditions.
2. Payers will always have to balance competing priorities: access and sustainability
Like providers, payers perform a balancing act between offering broad access to the greatest number of people and trying to sustain the system.
Ideally, they want to steer patients toward providers they know and trust. This helps keep costs down by limiting the most expensive care, for example readmissions for chronic disease. Patients, however, generally want freedom to choose providers they like; and so a tug of war ensues.
We have never seen payers hold so much power as they do now, especially with large health systems beginning to offer their own health plans and Medicare Advantage plans.
Under normal circumstances, the system works for healthy people. They can get routine and emergency care — and pay for it — under one roof; however, this also leads to fewer choices and less competition, which historically only drives up costs over time.
3. Payers will always try to get closer to the point of care
As we just laid out, the greatest example of this is when health systems have their own health plans.
But there can be other more nuanced ways for payers to influence the point — and cost — of care. Short of full-scale vertical integration, payers have the potential to engage in their own care management efforts to help improve patient outcomes and reduce risk.
This kind of engagement — going beyond the transactional nature of insurance — has been happening for decades, but it has never consistently worked to improve patient experience, quality of care and/or lower total costs because it ignores the one constant since the beginning of health care: patients trust their providers.
For any care management strategy to be successful, it must be implemented as an extension of the provider, not the payer.
4. Private payers will follow CMS
How closely and in what ways vary, but private payers and the Centers for Medicare and Medicaid Services are locked in an eternal dance. At a foundational level, private payer rates are based on a percentage of the Medicare rate. Therefore, when Medicare adjusts, the entire industry pays attention.
They don’t always match steps, but the kind of commanding power CMS has over private payers through this singular mechanism likely won’t change, as we see in this 2017 article about CMS’ understated influence on private payers.
5. Fees and networks will continue to frustrate patients
This is a result of the fragmented health system we’ve discussed in the other two parts of this series (see What Won’t Change? Part One: Patient Experience and What Won’t Change? Part Two: Provider Experience). Narrow networks will continue to separate patients from their providers of choice.
A new interim rule from the Department of Health and Human Services gives patients a little more confidence when seeking care that may or may not be in-network, especially in the emergency department and operating room where several providers with inconsistent network affiliations deliver care to the same person.
Payers don’t have agreements with all providers, which inevitably means some doctors will always be out of reach for some patients.
What do we take from the persistent parts of payer experience?
The desire to control costs links together all of the payer experience mainstays.
As a chronic care management company, Signallamp Health understands how routine maintenance for the sickest patient segments drives down expenditures while making care more sustainable and accessible for a greater number of people.
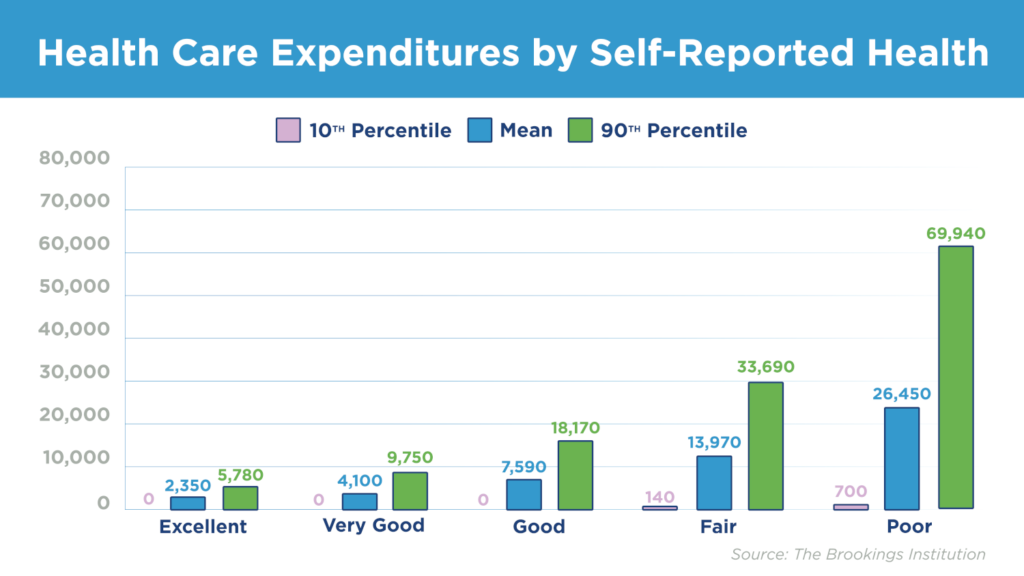
Of people in poor health, the top 90th percentile accounts for 100 times the annual spending compared to people in the 10th percentile, according to the Brookings Institution report we mentioned at the top. That’s the difference between $700 and $70,000 annually.
Signallamp thrives in this part of the patient continuum.
Through routine longitudinal case management and routine telephone check-ins, we’re systematically reducing acute medical incidents and helping patients achieve their highest level of wellbeing.
Insurance companies will always struggle to balance sustainability and access. At Signallamp Health, we bring value to providers and help them achieve both. Schedule a consultation to find out how.