
These elements of the patient experience aren’t likely to change in the next 10 years
This is the first of a three-part series called “What Won’t Change?” where we examine the mainstays in health care that are likely to stay the same over the next decade.
1. The elderly population will continue to grow
Health care is extending lifetimes, but does that mean quality of life is following suit? Our life expectancy is as high as it’s ever been historically speaking (dips these past few years are a notable exception), which sounds great.
But extending life does not necessarily mean extending the same quality of life. Health care providers will continue to be challenged to not only extend lifetimes, but also preserve quality of life.
At this point, the tail end of the enormous baby boomer generation is approaching retirement age, which means people in the second largest generation — about 65 million people in the U.S. — are consuming more health care than they ever have.
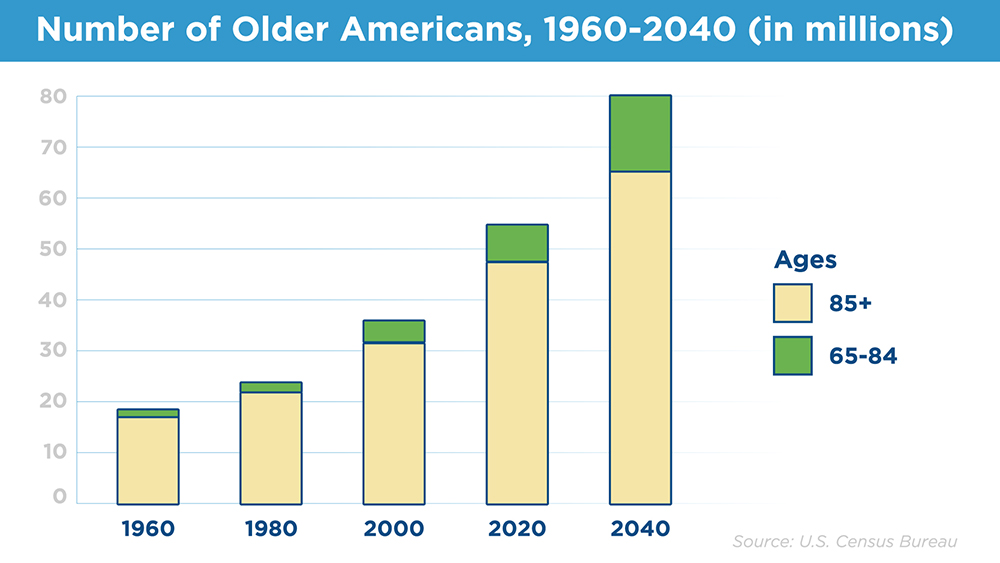
The older population is only expanding. Using census data, the Urban Institute predicts people aged 65 and older will number 80 million by 2040. At that time, older populations are estimated to include their largest share of people over the age of 85, around 15 million.
2. Chronic disease continues
Persistence is the hallmark of chronic illness. As patients age, they’re more likely to pick up chronic illnesses over time, and then keep them forever.
There’s no perfect way to predict chronic disease incidence; however, the Centers for Disease Control and Prevention says 78% of men and women 55 and older have one or more chronic diseases. Since chronic illness isn’t like a virus or other infection, and more related to the status of our physiology, we expect these rates to remain fairly consistent.
In even older brackets, it becomes even more prevalent. About 86% of people 65 and older have at least one chronic condition, the CDC says.
Chronic disease is not inevitable, and through lifestyle adjustments and good habits, many people can avoid them. That said, we can reasonably expect that with an aging population, so too will chronic disease incidence become more prevalent.
3. People will move less because of technology
The convenience and connectivity of the internet present a sinister tradeoff. When movement is optional, some people are going to opt out because physical activity takes intention and work. That’s human nature.
An extensive study published in 2019 in the Journal of the American Medical Association found that between 2003 and 2016, computer use of an hour or more per day, outside school or work, increased significantly in all age groups. Presumably, the authors concluded, these people were sedentary when they could have otherwise been physically active.
Among adults in that group — people who use a computer outside of work or school for more than one hour per day — their numbers grew from 29% of the population to a stunning 50% in that time period. The greatest increment was among people 65 and older.
When people move less, it leads to or exacerbates more chronic disease. Inactive lifestyles are factors for most chronic diseases including but not limited to diabetes, COPD, cancer, hypertension and heart failure.
The need to maintain activity will always go hand-in-hand with new technology developed for convenience.
On the other hand, we have troves of data that shows technology can help us move more. Fitness trackers and gamifying physical activity have shown to be incredibly effective at getting people to move more.
The trick will be making sure we balance the convenience with incentives to move.
4. Nutritious and affordable food will continue to be harder to find
Along with the diminishing need to get up and move, fresh, nutritious food has always been on the margins of the grocery store. Meanwhile, all the packaged stuff is conveniently in the middle. Supermarkets in wealthier communities have bursting produce sections right inside the font door. In poorer or more remote communities, a convenience or discount store is often the only grocery option.
Packaged foods will almost always:
- Be more cost accessible
- Have higher processed sugar content and more additives
- Have less fiber and other important nutrients
- Taste better right out of the package
- Require less prep time
- Come more shelf-stable and easier to store
- Have preferred placement in grocery stores alternatives
5. Patients are human and will continue to stray off course
We humans undulate when it comes to self care. We’ll exercise for a few months, then drop off. We stick to wholesome diets, then completely abandon them. We quit smoking, drink less alcohol, then stumble back into addiction again.
Generally speaking, heading in the right direction with a little backsliding is OK. But for people with chronic illness, a relapse into bad habits can be dangerous.
As a chronic care management provider, Signallamp Health nurses provide an invaluable framework that supports good habit formation (and eliminating the bad ones). We know staying on course gets a lot easier when we have a support system to keep us there.
6. Patients will continue to get care in fragmented ways
A patient’s primary care doc has slightly different priorities than their specialists. While providers can view shared records through an electronic medical record, they do it through different lenses, and then deliver care based on their interpretations.
Electronic systems will get better at sharing patient records safely and reliably, but patients will almost certainly fall through the cracks or experience redundancy when receiving care across disciplines.
Added to this, patients usually meet with their providers or specialists just a few times per year. Given chronic disease is a part of their daily lives, connecting with patients regularly in between those visits is critical to ensure they manage their diseases effectively and that early intervention happens when needed to prevent emergency room visits and hospitalizations.
An effective chronic care management system fills the gaps and coordinates care between specialists and primary care providers. With CCM, patients have dedicated advocates who understand their complex health needs. In addition, nurse case managers know when to speak up when care delivery falls out of sync between providers.
7. The way people form meaningful relationships won’t change
Patients are people. And as much as people get a dopamine kick out of swiping through a dating app or endless scrolling on TikTok, truly meaningful relationships involve facetime and high-touch interactions.
When it comes to maintaining the patient experience, more direct interactions will lead to more accountability, more satisfied patients and better outcomes. That won’t change.
What does all this mean?
Ultimately, if most or all of these patient elements remain the same over the next 10 years, extending your relationship with your patients beyond your offices and hospitals, and engaging them longitudinally with care management resources, is an absolute necessity to be successful at improving outcomes and lowering costs.
At Signallamp Health, we understand that the patient experience includes some immovable mainstays. Instead of treating them like obstacles, we treat them like opportunities. Schedule a consultation with us to find out how.

