4 Critical Steps to Successful CCM Implementation
Successful chronic care management implementation takes many coordinated steps. Each requires people, time and infrastructure, but that’s just the starting point.
At Signallamp Health, we’ve streamlined the implementation process to quickly scale up CCM programs for providers and health systems. We’ve worked out all the bugs so you don’t have to.
We’ve also identified four critical steps to successful implementation that you might consider extra or as part of a wish list. But take our advice: a successful CCM program absolutely needs these four steps. Otherwise, outcomes will fail to measure up to your goals.
Step 1: Master Recruitment and Training Processes
To achieve true scale, you must enroll at least half of your eligible patient population.
In order to reach those enrollment numbers, you need robust recruiting and a strong training infrastructure.
On the recruiting side, you need to clearly define the kind of talent required. It’s one thing to have a list of must-haves for your recruiters to lay out in a job posting. It’s another thing entirely to have knowledgeable recruiters who can identify good candidates for the remote work setting. Eligible remote nurses should have the right kind of experience, a strong, self-empowered work ethic and the ability to work from home.
At Signallamp Health, our recruiters are also the same nurses who make up our quality team. Signallamp’s team of nurses can spot these traits from a mile away. Since that’s all they do, they understand the type of nurse who thrives in a remote environment and forge true connections with patients. They understand how to incentivize capable nurses to join the team — and stay on the team.
It goes without saying that retention is also part of this step. Consistency is a key component of any successful CCM program because nurses build meaningful relationships with their patients, which improve outcomes. Health care, after all, is still an utterly human craft.
Once the workforce is in place, nurses complete training with a focus on quality patient care. Workflows must align with the best patient outcomes. Nurses have to maximize productivity while finding the time required to deliver quality care.
Signallamp nurse managers understand which key performance indicators to track in order to satisfy those two goals — productivity and time with patients — which notoriously run against each other unless properly managed.
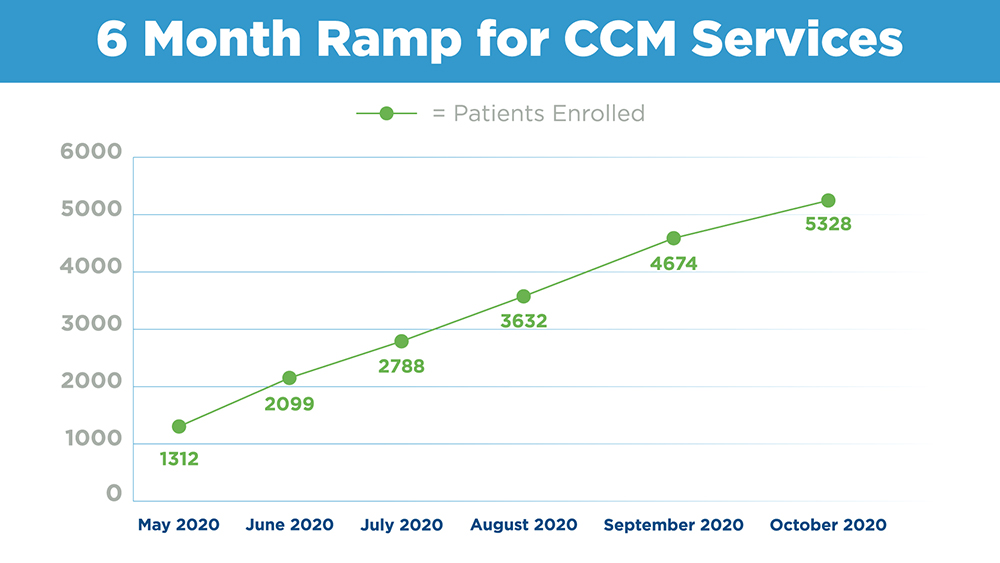
The graph below shows enrollment data taken from an actual Signallamp client implementation. Without a solid recruiting and training process, the Signallamp nurse care team embedded with the client could have never kept up with the pace of our enrollment team.
Step 2: Separate Enrollment and Care Teams
This one seems obvious, but in a pinch, might be the first corner providers try to cut to the detriment of the whole program. It comes down to one axiom:
Nurses provide care; they are not salespeople.
Nurses tasked with enrollment waste their talent and training to onboard new patients. Enrollment requires an entirely different skillset.
By allowing nurses to focus on delivering quality care, it keeps the focus on patients.
Step 3: Nurses Should Work with the Same Providers and Patients
We mentioned continuity in Step 1. Here’s why it’s important.
Human relationships engender patient engagement. Patient engagement leads to better outcomes. We don’t need to explain that one. Scientists have explored the relationship between engagement and outcomes for decades with results resoundingly pointing in the same direction.
Signallamp remote nurses engage with the same doctors and their patients month after month. They integrate fully with providers’ electronic medical records enabling seamless communication and recordkeeping.
They also form powerful, trusting relationships with patients through monthly telephone check-ins. Patients reveal new information about symptoms or health concerns to their Signallamp nurses. Those check-ins provide an anchor for patients and a gentle reminder to keep their care top-of-mind.
Step 4: Educate Providers and Staff
This might be one of the most complicated, but also most important of the steps.
Care teams, including providers and clinical staff, must advocate for the chronic care management program. They must understand the program, believe in its purpose and champion enrollment. Success starts with buy-in from everyone who will be utilizing and implementing the program.
Signallamp supplies each provider with training and leave-behind materials so they can, in turn, educate their patients about the value, and the better health and wellness that come with an effective CCM program.
Successful Chronic Care Management Starts with the Right Partner
The truth remains, health systems and provider groups categorically struggle to build out their own chronic care management infrastructure in-house. Virtually no health system in the U.S. has enrolled more than 5% of its eligible population. It’s not easy, and as we described in these four critical steps, takes a high level of expertise and infrastructure.
Even the nation’s most established health systems, like UPMC, Temple and Sinai have learned that, through a strategic partnership with Signallamp Health, CCM can scale and flourish at a meaningful pace. It can produce profound new outcomes.
Signallamp Health helps you master these four critical steps and achieve a scale previously unattainable within your CCM program.

