2020 Medicare Chronic Care Management CPT Codes Simplified
First, what is Chronic Care Management (CCM)?
The Centers for Medicare & Medicaid Services (CMS) defines CCM services as those provided by a physician, PA, NP, clinical nurse specialist, or certified nurse midwife and their clinical staff, per month, for patients with two or more chronic conditions expected to last at least 12 months or until death, and that place the patient at significant risk of death, acute exacerbation or functional decline. These services can be delivered in-person or over the phone.
What are the current billable CPT codes for chronic care management services in 2020?


In 2020, there are currently three main CPT codes and two add-on CPT codes that can be billed by primary care practices for chronic care management services. These are as follows:
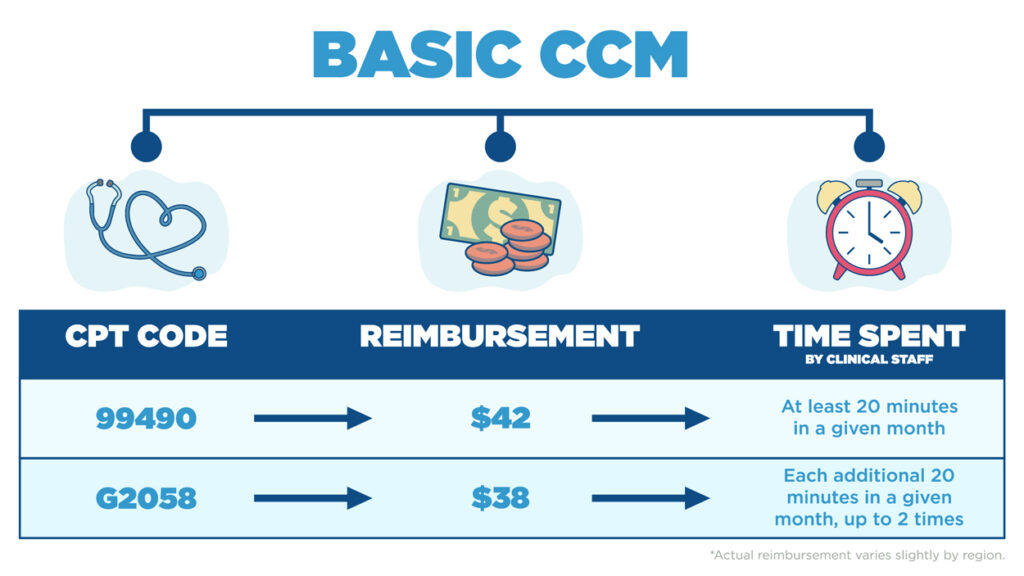
For the basic CCM CPT code 99490, patients must have two or more chronic conditions, as well as documented consent to enroll in the program AND receive at least 20 minutes of CCM services from clinical staff within a given month. A personalized care plan, which shows an assessment of all patient factors and identifies gaps and barriers to be addressed, must also be created and provided to the patient. The add-on code for basic CCM is G2058. It allows for billing for each additional 20 minutes of time spent for basic CCM services in a given month, up to 2 times. For example, if CCM services were provided for at least 40 minutes with a patient in a given month that was not complex, 99490 ($42) and G2058 ($38) would be billed together for that month.
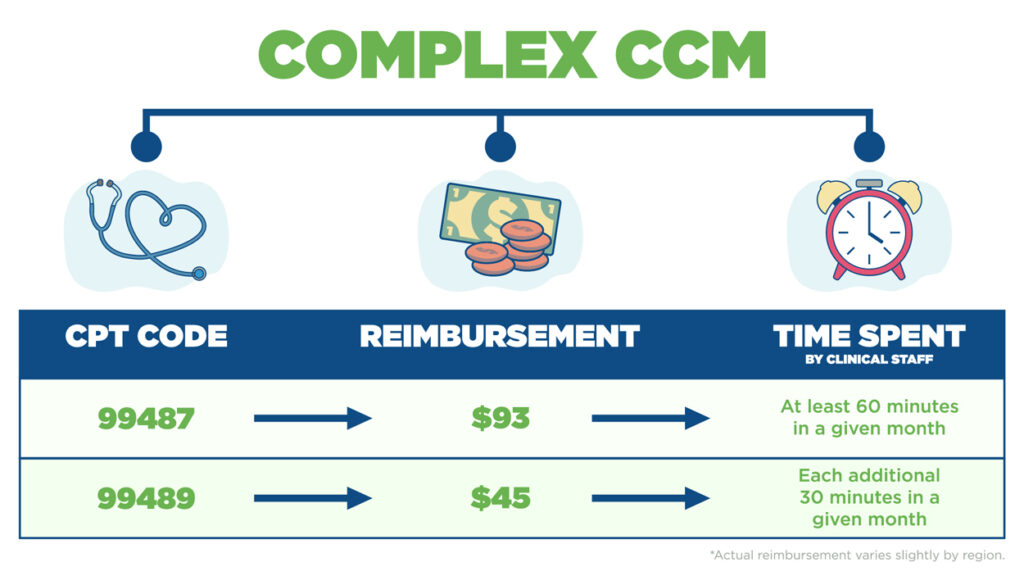
For your complex patients, CMS offers CPT code 99487, which has a higher rate of reimbursement than the basic CCM CPT code. To bill using this code requires moderate or high complexity in medical decision making and acknowledgement of both patient & provider of an acute exacerbation. Patient must receive at least 60 minutes of services from clinical staff within a given month. An acute exacerbation is generally defined as a sudden worsening of a patient's condition that necessitates additional time and resources. Just like with the basic CCM code, the complex CCM code also has an add-on code to cover time spent beyond 60 minutes. That CPT code is 99489. It allows for billing for each additional 30 minutes of time spent for complex CCM services within a given month. For example, if 90 minutes of clinical services is provided to a patient in a given month that was complex, they would bill 99487 ($93) and 99489 ($45) for that month.
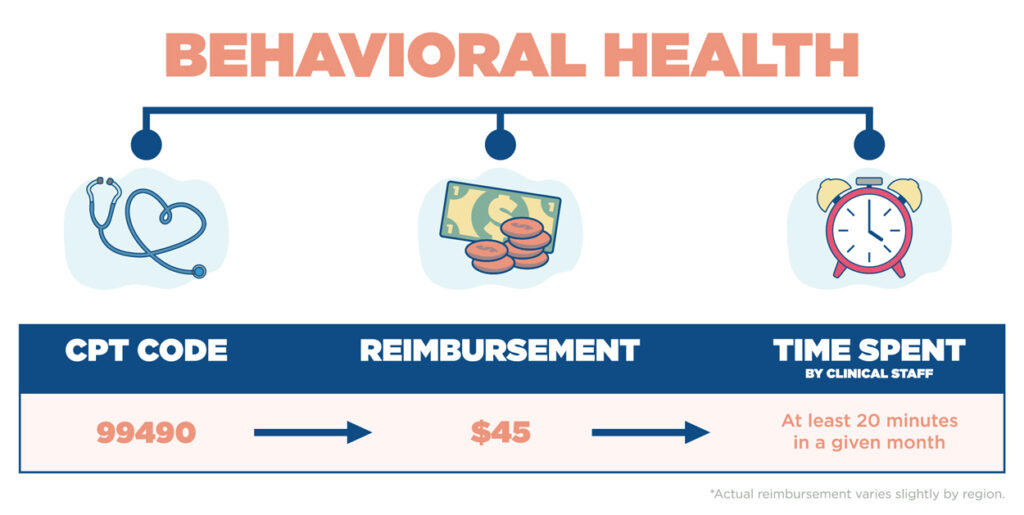
In addition to basic and complex chronic care management CPT codes, CMS also offers one behavioral health CPT code for primary care practices to bill for behavioral health services. That CPT code is 99484, which is for Behavioral Health Integration. This is the only behavioral health code that can be fully supported by a primary care practice. To qualify, the patient must have at least one behavioral health condition and receive at least 20 minutes of Behavioral Health Integration (BHI) services from clinical staff each month. It also requires a separate enrollment & consent form and care plan.
Click below to consult with us on how we can help you to create a self-sustaining chronic care management program that drives bottom line revenue and improves patient outcomes.
